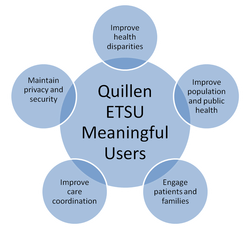
· Improve quality, safety, efficiency, and reduce health disparities,
· Engage patients and families in their healthcare,
· Improve care coordination,
· Improve population and public health, and
· Maintain privacy and security.
Remarkably, we have already seen first-hand examples of Quillen ETSU providers and clinical staff using our EHR to each of these ends.
Addressing health disparities has been the primary focus of the patient lists generated for each provider. Many of the family medicine and internal medicine providers now have access to a list of all their diabetic patients with records in the EHR.
These lists help providers and clinics manage this patient population, who, in Tennessee, had a 19% higher risk of dying from diabetes than the national average. The Tennessee diabetes death rate of 30.2 per 100,000 was ranked 10th highest in the nation in 2002. In 2004, the age-adjusted diabetes death rate for black Tennesseans (61.1 per 100,000) was over twice the rate for whites (27.8 per 100,000).*
*Information from tn.gov.

As we look toward adding a patient portal, patients will gain even more access to their health records, and, hopefully, this will prompt many of them to become more engaged in their own healthcare.
Improving care coordination has been one of the biggest benefits of using the system. With multiple providers and specialties having quick access to the patient’s chart, duplicate labs and medications have significantly decreased, saving patients money and time.
The referral process to providers within ETSU clinics has also been significantly improved. Faxing records is no longer necessary, and clinics can use tasking rather than phones and faxing to make the referral.
With the system’s ability to track and report data, we are now able to run reports on various population and public health initiatives. In the Department of Pediatrics, data has been requested to track abnormal labs, the Read N Play initiative, and reflux diagnoses. In the Department of Family Medicine, various information is being tracked for improvement of their Patient-Centered Medical Home designation, as well as monthly reports on Controlled Substance prescriptions.
The system is also designed to generate reminders based on either input from individual providers or as system-generated reminders based on recommended screening and diagnostic guidelines, such as colorectal cancer and mammography screenings. Recently, reminders have been set up for CSMD checking for patients on controlled substance prescriptions.
Maintaining privacy and security has always been a top concern for EHR users, no matter what the system. With retail electronic security breaches being reported regularly, many healthcare providers questioned the security of electronic health records when EHR systems were first introduced into practices. However, with quickly evolving technologies, and the stringent requirements on systems in order to be certified for Stage 1 of Meaningful Use, EHR systems are exceptionally secure. Eligible providers need to “attest” that they have met certain measures or requirements regarding the use of the EHR for patient care.
EHRs are more secure than most paper charts ever were, especially within organizations where chart audits are frequently performed. In the paper world, if an employee wanted to access a health record without reason, most likely, no one would ever know if he or she had been in the record. With electronic records, anyone who accesses a chart is trackable, resulting in a more secure health record.
As we all become better users, the possibilities for how the system can be used in more meaningful ways will be illuminated.



 RSS Feed
RSS Feed