
So, if Stage 2 is the villian, guess who gets to be the superhero?
Let’s start by taking Uncle Ben’s advice, “With great power comes great responsibility.” And the first responsibility you’ll have as “MU Man” or “MU Woman” is learning everything you can about the requirements for attestation.
We will soon be posting a training presentation (eligible for CME credit) which will detail what and how to document the Stage 2 requirements, but as a quick summary, below are the 17 core measures and 3 menu measures that are required for Stage 2.
Stage 2 Core and Menu Measures
Core Objectives (17 total)
(1) Use computerized provider order entry (CPOE) for medication (>60%), laboratory (>30%) and radiology orders (>30%) directly entered by any licensed healthcare professional who can enter orders into the medical record per state, local, and professional guidelines.
(2) Generate and transmit permissible prescriptions electronically (>50%).
(3) Record the following demographics: preferred language, sex, race, ethnicity, and date of birth (>80%).
(4) Record and chart changes in the following vital signs: height/length and weight (no age limit); blood pressure (ages 3 and over); calculate and display body mass index (BMI); and plot and display growth charts for patients 0-20 years, including BMI (>80%).
(5) Record smoking status for patients 13 years old or older (>80%).
(6) Use 5 clinical decision support interventions to improve performance on high-priority health conditions (these must be related to Clinical Quality Measures) AND enable and implement drug-drug and drug-allergy checks.
(7) Provide patients the ability to view online, download, and transmit their health information within four business days of the information being available to the EP (>50%).
(8) Provide clinical summaries for patients for each office visit (>50%).
(9) Protect electronic health information created or maintained by the Certified EHR Technology through the implementation of appropriate technical capabilities.
(10) Incorporate clinical lab-test results into Certified EHR Technology as structured data (>55%).
(11) Generate lists of patients by specific conditions to use for quality improvement, reduction of disparities, research, or outreach.
(12) Use clinically relevant information to identify patients who should receive reminders for preventive/follow-up care and send these patients the reminders, per patient preference (>10%).
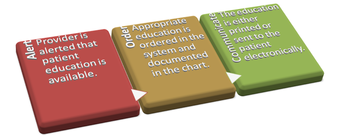
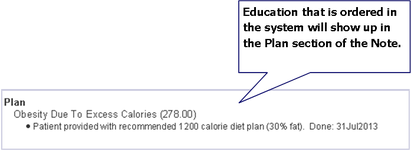
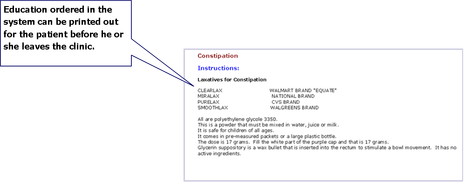
(13) Use clinically relevant information from Certified EHR Technology to identify patient-specific education resources and provide those resources to the patient (>10%).
(14) The EP who receives a patient from another setting of care or provider of care or believes an encounter is relevant should perform medication reconciliation.
(15) The EP who transitions their patient to another setting of care or provider of care or refers their patient to another provider of care should provide a summary care record for each transition of care or referral (>50%).(16) Capability to submit electronic data to immunization registries or immunization information systems except where prohibited, and in accordance with applicable law and practice (Yes/No).
(17) Use secure electronic messaging to communicate with patients on relevant health information (>5%).
Eligible Professional Menu Objectives (3 of 6)
(1) Record electronic notes in patient records (>30%).
(2) Imaging results consisting of the image itself and any explanation or other accompanying information are accessible through CEHRT (>10%).
(3) Record patient family health history (1st degree relative) as structured data (>20%) .
If you’re still learning the ropes on how to use your superpowers (a.k.a. EHR documentation skills), this Stage 2 summary may have you rethinking your superhero status, but no one ever promised saving the world was easy.
And I haven’t even mentioned CQMs!












 RSS Feed
RSS Feed