
So exactly what have I learned?
1. Computers can be glitchy, but they provide a lot of valuable information. While at the hospital and at follow-up appointments with Anna, there were a few times that the computers froze or caused a problem, but, honestly, not that often. And given the alternative —of not having Anna’s information readily available and having to wait on records to be faxed—I’ll take the occasional glitch. Anna has seen multiple providers during the past few months, and with all them having access to her electronic chart, it put my mind at ease.
2. Computers do get in between the provider and patient, but it isn’t all that bad. I have heard several clinicians say that they feel like the computer gets in between them and the patient. And I have also heard patients say the same thing. But from what I observed during Anna’s experience, it’s not really that intrusive. Sure, you have to spend some time entering information, but once the information was entered, all of her providers spent time examining her and talking to her directly. It definitely wasn’t any different than writing down the information on paper. I discovered that most everyone who saw her has developed a balance in using the computer and seeing the patient.
3. An EHR saves the patient money. As mentioned in #1 above, when providers share the same record, it’s time gained, but it’s also money saved. All of Anna’s orders (labs, imaging, etc.) were shared by all of her providers, and no duplicate tests were unnecessarily ordered, saving me money.
4. The Clinical Summary is nice. First of all, let me say that Crystal, one of the check-in staff at Pediatrics, does an awesome job. She never forgot to ask us if we wanted a clinical summary of our visit. Although I didn’t need her to print it for all of Anna’s visits, the document has come in handy at other times. With so many medications and orders and diagnoses, it’s difficult to keep track of all that information, especially during a stressful acute illness. Thank you, Crystal, for always asking, because there are times when this mom forgets things.
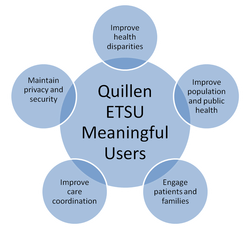
5. Quillen ETSU Physicians are wonderful physicians. Although I’ve taken advantage of Anna’s illness for inspiration to write, I hope everyone will indulge me. The most valuable perspective I gained during this experience is how wonderful our physicians and staff are. Anna has received the best of care, and I can’t say enough how appreciative I am for everyone who has helped her. To everyone at ETSU Family Medicine in Johnson City, ETSU Pediatrics, and ETSU Surgery, thank you so much for providing the best of care. You rock (the EHR, too)!

 RSS Feed
RSS Feed